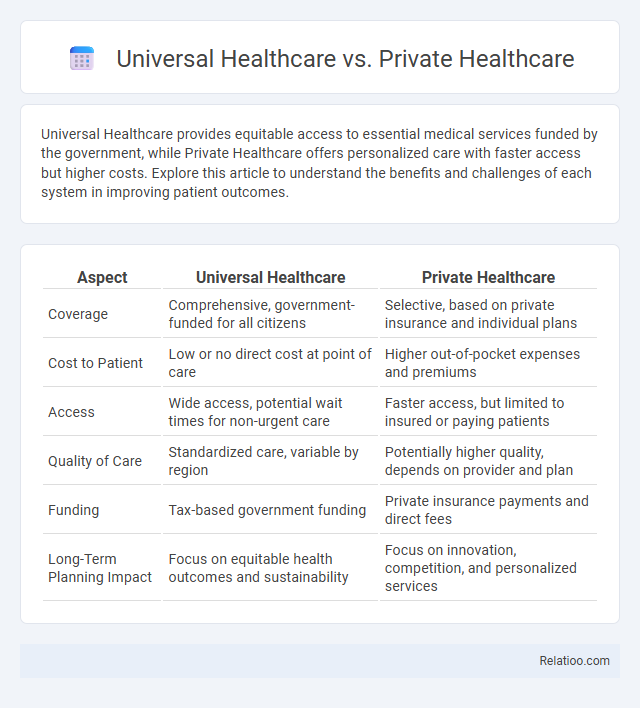
Universal Healthcare provides equitable access to essential medical services funded by the government, while Private Healthcare offers personalized care with faster access but higher costs. Explore this article to understand the benefits and challenges of each system in improving patient outcomes.
Table of Comparison
| Aspect | Universal Healthcare | Private Healthcare |
|---|---|---|
| Coverage | Comprehensive, government-funded for all citizens | Selective, based on private insurance and individual plans |
| Cost to Patient | Low or no direct cost at point of care | Higher out-of-pocket expenses and premiums |
| Access | Wide access, potential wait times for non-urgent care | Faster access, but limited to insured or paying patients |
| Quality of Care | Standardized care, variable by region | Potentially higher quality, depends on provider and plan |
| Funding | Tax-based government funding | Private insurance payments and direct fees |
| Long-Term Planning Impact | Focus on equitable health outcomes and sustainability | Focus on innovation, competition, and personalized services |
Introduction to Universal and Private Healthcare
Universal healthcare provides comprehensive medical services accessible to all citizens, funded primarily through taxation, ensuring equitable access regardless of income. Private healthcare operates on a user-pay model, offering faster service and specialized treatments, but often at higher out-of-pocket costs, creating disparities in care availability. Understanding your healthcare options enables informed decisions tailored to your medical needs and financial situation.
Historical Overview of Healthcare Systems
The evolution of healthcare systems reflects shifting societal priorities and economic models, with universal healthcare emerging in the early 20th century through landmark policies like the UK's National Health Service established in 1948, emphasizing equitable access to medical services funded by taxation. Private healthcare, with roots in 19th-century Europe and the United States, developed alongside industrialization, driven by market-based approaches and health insurance companies offering personalized care options. Health planning gained prominence in the mid-20th century as governments recognized the need for systematic resource allocation and long-term strategies to address public health challenges and improve overall population outcomes.
Accessibility and Coverage: Who Gets Care?
Universal healthcare ensures that all individuals have access to essential medical services regardless of income, significantly reducing disparities in coverage. Private healthcare often provides faster access and more personalized care but can limit accessibility based on insurance status or financial means. Your ability to receive timely and comprehensive care largely depends on whether the system prioritizes universal coverage or relies on private healthcare infrastructure and personal health planning.
Cost to Individuals: Out-of-Pocket vs. Tax Funded
Universal healthcare minimizes your out-of-pocket expenses by primarily funding services through taxes, ensuring broad access regardless of personal income. Private healthcare generally requires higher direct payments or insurance premiums, placing a larger financial burden on individuals. Effective health planning balances these models to optimize cost efficiency and access, reducing unexpected medical expenses while leveraging public funding.
Quality of Healthcare Services
Universal healthcare ensures equitable access to essential medical services, often resulting in consistent quality standards through government regulation and funding. Private healthcare typically offers personalized care with shorter wait times and advanced technology, but quality can vary significantly based on provider and insurance coverage. Health planning integrates both systems by strategically allocating resources and coordinating care to optimize quality outcomes and address population-specific needs.
Wait Times and Efficiency
Universal healthcare systems tend to offer more equitable access but often face longer wait times due to higher patient volumes and resource constraints. Private healthcare typically provides quicker access to specialized treatments and shorter wait times by leveraging greater efficiency and investment in technology and staffing. Effective health planning, including resource allocation and demand forecasting, is critical to optimizing wait times and improving the overall efficiency of both universal and private healthcare systems.
Health Outcomes and Population Well-being
Universal healthcare systems demonstrate superior health outcomes and population well-being by providing equitable access to essential services, reducing disparities in care, and improving preventive measures. In contrast, private healthcare often leads to variable health outcomes due to cost barriers and unequal service availability, limiting comprehensive disease prevention and management. Strategic health planning integrates data-driven policy and resource allocation, enhancing both universal and private systems by optimizing service delivery and addressing population-specific health needs efficiently.
Impact on Medical Innovation
Universal healthcare systems often prioritize broad access and cost-efficiency, which can limit funding for cutting-edge medical innovation compared to private healthcare models that incentivize rapid development through market competition. Private healthcare drives innovation by investing heavily in research and development, focusing on breakthrough technologies and personalized treatments that push medical boundaries. Your choice between these systems influences how quickly new medical advancements become available and affordable in your region.
Equity and Social Justice in Healthcare
Universal healthcare ensures equitable access to essential medical services regardless of income, promoting social justice by reducing health disparities among marginalized populations. Private healthcare often prioritizes profit, leading to unequal treatment access and exacerbating health inequities for low-income individuals. Your commitment to health planning can bridge gaps by integrating policies that emphasize equity, ensuring fair distribution of resources and improving outcomes for all societal groups.
Future Trends and Policy Considerations
Universal healthcare systems emphasize equitable access and cost containment, with future trends focusing on integrating digital health technologies and value-based care models to enhance population health outcomes. Private healthcare continues to drive innovation and personalized services, but faces policy challenges around affordability and regulatory alignment to ensure equitable access without sacrificing quality. Health planning increasingly incorporates data analytics and predictive modeling to optimize resource allocation, prioritize preventive care, and address demographic shifts, necessitating policy frameworks that balance technological adoption with ethical and social considerations.
Infographic: Universal Healthcare vs Private Healthcare
 relatioo.com
relatioo.com