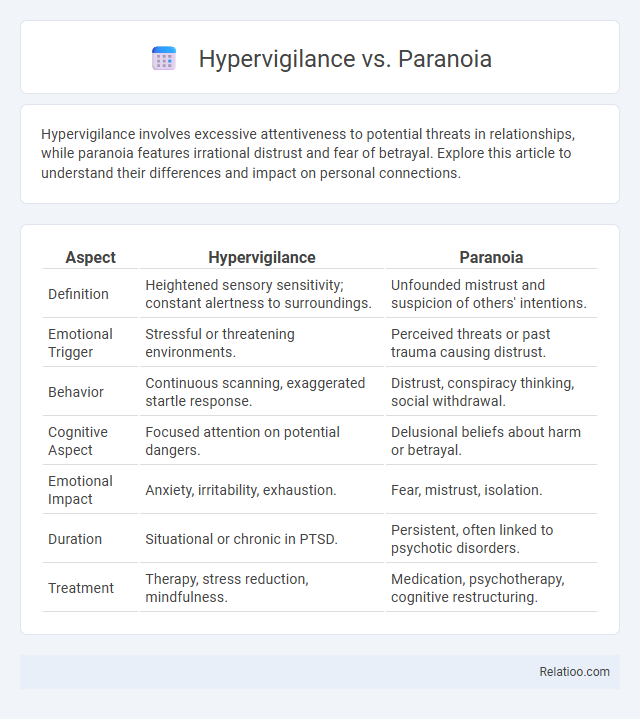
Hypervigilance involves excessive attentiveness to potential threats in relationships, while paranoia features irrational distrust and fear of betrayal. Explore this article to understand their differences and impact on personal connections.
Table of Comparison
| Aspect | Hypervigilance | Paranoia |
|---|---|---|
| Definition | Heightened sensory sensitivity; constant alertness to surroundings. | Unfounded mistrust and suspicion of others' intentions. |
| Emotional Trigger | Stressful or threatening environments. | Perceived threats or past trauma causing distrust. |
| Behavior | Continuous scanning, exaggerated startle response. | Distrust, conspiracy thinking, social withdrawal. |
| Cognitive Aspect | Focused attention on potential dangers. | Delusional beliefs about harm or betrayal. |
| Emotional Impact | Anxiety, irritability, exhaustion. | Fear, mistrust, isolation. |
| Duration | Situational or chronic in PTSD. | Persistent, often linked to psychotic disorders. |
| Treatment | Therapy, stress reduction, mindfulness. | Medication, psychotherapy, cognitive restructuring. |
Understanding Hypervigilance: Definition and Symptoms
Hypervigilance is an enhanced state of sensory sensitivity accompanied by an exaggerated intensity of behaviors aimed at detecting threats, often linked to trauma or anxiety disorders. Symptoms include being easily startled, constantly scanning the environment for danger, and difficulty concentrating due to persistent alertness. Understanding these signs can help you differentiate hypervigilance from paranoia, which involves unfounded fears or beliefs of being targeted, whereas hypervigilance is a genuine heightened awareness.
What is Paranoia? Key Signs and Features
Paranoia is characterized by intense, irrational distrust and suspicion of others without sufficient evidence, often leading to feelings of persecution. Key signs include persistent fear that others have malicious intentions, misinterpretation of neutral events as threatening, and difficulties in social relationships due to suspicion. Unlike hypervigilance, which involves heightened sensory awareness often linked to anxiety or trauma, paranoia centers on distorted thoughts and beliefs about others' intentions.
Causes of Hypervigilance: Trauma, Anxiety, and Beyond
Hypervigilance often stems from trauma, anxiety disorders, or chronic stress, causing heightened sensory sensitivity and constant alertness to potential threats. Distinct from paranoia, which involves irrational suspicion, hypervigilance is a response developed from real or perceived danger, helping your brain anticipate and respond to threats more quickly. Understanding these causes enables targeted strategies to manage symptoms and reduce the overwhelming state of alertness.
Underlying Factors Leading to Paranoia
Paranoia often stems from complex underlying factors such as past trauma, chronic stress, or neurochemical imbalances affecting the brain's threat assessment systems. Unlike hypervigilance, which is characterized by heightened sensory sensitivity and a focus on environmental cues for safety, paranoia involves persistent irrational mistrust and beliefs not grounded in reality. Understanding the neurological and psychological triggers, including amygdala hyperactivity and dopamine dysregulation, is crucial for distinguishing paranoia from closely related conditions like hypervigilance.
Hypervigilance vs Paranoia: Core Differences
Hypervigilance involves an enhanced state of sensory sensitivity and constant scanning of the environment for potential threats, often linked to anxiety disorders or PTSD, whereas paranoia is characterized by irrational and persistent mistrust or suspicion of others' motives without sufficient evidence. Your ability to distinguish between hypervigilance and paranoia hinges on recognizing that hypervigilance is a heightened alertness based on real or perceived danger, while paranoia entails delusional fears that others intend harm. Understanding this core difference aids in identifying appropriate mental health interventions tailored to each condition's underlying causes.
Impact on Daily Life: Hypervigilance compared to Paranoia
Hypervigilance often results in constant scanning of the environment for threats, leading to heightened anxiety and difficulty concentrating on routine tasks, which disrupts daily functioning. Paranoia involves persistent mistrust and irrational beliefs about others' intentions, causing social withdrawal and impaired relationships. While hypervigilance primarily affects alertness and stress levels, paranoia more profoundly impacts social interactions and emotional well-being.
Diagnosis Challenges: Overlapping and Distinctive Symptoms
Hypervigilance, paranoia, and hyperawareness share overlapping symptoms like heightened alertness and suspicion, complicating accurate diagnosis. Distinctive features help differentiate them: hypervigilance often relates to trauma reactions with exaggerated sensory sensitivity, paranoia involves irrational mistrust or delusions, and hyperawareness centers on an intense focus on bodily sensations. Clear clinical assessment focusing on symptom patterns and patient history is essential for correctly identifying your condition and providing effective treatment.
Treatment Approaches for Hypervigilance
Treatment approaches for hypervigilance primarily involve cognitive-behavioral therapy (CBT) to help individuals recognize and modify excessive alertness and anxiety triggers. Pharmacological interventions, such as selective serotonin reuptake inhibitors (SSRIs) or benzodiazepines, may be prescribed to manage underlying anxiety or PTSD symptoms contributing to hypervigilance. Mindfulness-based stress reduction and relaxation techniques further support reducing the constant state of heightened sensory sensitivity characteristic of hypervigilance.
Managing Paranoia: Effective Therapies and Strategies
Managing paranoia effectively involves cognitive-behavioral therapy (CBT), which helps you identify and challenge irrational thoughts while building coping mechanisms. Medications such as antipsychotics can reduce paranoia symptoms, especially when linked to underlying mental health conditions like schizophrenia. Incorporating stress reduction techniques, mindfulness, and strong social support further enhances treatment outcomes and helps distinguish paranoia from hypervigilance, which is excessive alertness without the persistent suspicious beliefs characteristic of paranoia.
Seeking Help: When to Consult a Mental Health Professional
Recognizing when to seek help is crucial for managing hypervigilance, paranoia, and their overlap, as persistent symptoms may indicate underlying mental health disorders like anxiety, PTSD, or psychosis. You should consult a mental health professional if your heightened alertness or suspicious thoughts significantly interfere with daily functioning, relationships, or cause distress. Early intervention through therapy or medication can improve outcomes and help you regain control over your mental well-being.
Infographic: Hypervigilance vs Paranoia
 relatioo.com
relatioo.com