Isolation refers to a state of being physically or emotionally separated from others, often leading to feelings of loneliness and disconnection, while seclusion is a deliberate choice to withdraw from social interaction for reflection or rest. Understanding the impacts of isolation and seclusion on relationships can improve emotional well-being and communication; discover more insights in this article.
Table of Comparison
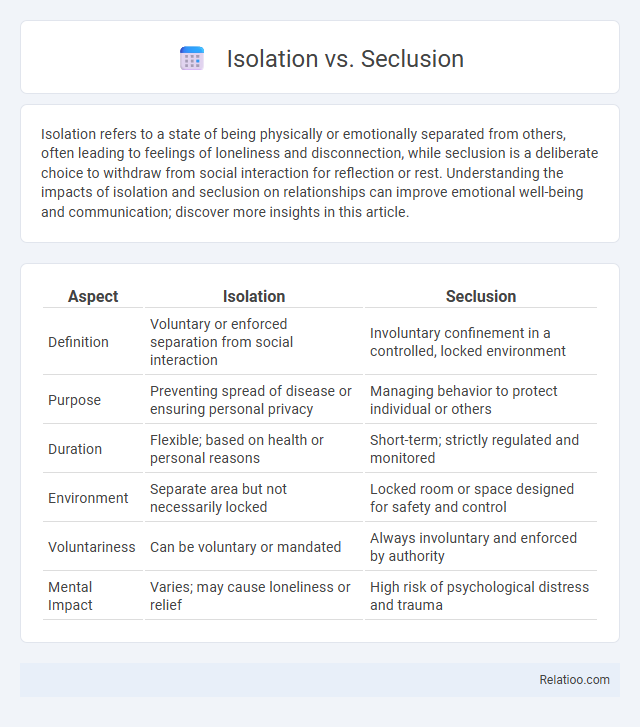
| Aspect | Isolation | Seclusion |
|---|---|---|
| Definition | Voluntary or enforced separation from social interaction | Involuntary confinement in a controlled, locked environment |
| Purpose | Preventing spread of disease or ensuring personal privacy | Managing behavior to protect individual or others |
| Duration | Flexible; based on health or personal reasons | Short-term; strictly regulated and monitored |
| Environment | Separate area but not necessarily locked | Locked room or space designed for safety and control |
| Voluntariness | Can be voluntary or mandated | Always involuntary and enforced by authority |
| Mental Impact | Varies; may cause loneliness or relief | High risk of psychological distress and trauma |
Understanding Isolation and Seclusion: Key Definitions
Isolation refers to the practice of separating an individual to prevent the spread of contagious diseases, often used in medical or infection control settings. Seclusion involves confining a person, usually in a controlled environment, to manage behavior and ensure safety, commonly applied in psychiatric or disciplinary contexts. Understanding the distinct purposes and applications of isolation and seclusion helps you make informed decisions about their appropriate use.
Historical Perspectives on Isolation and Seclusion
Historical perspectives on isolation and seclusion reveal their evolving roles in healthcare and social control, particularly in mental health treatment and contagion prevention. Isolation has traditionally referred to separating individuals with infectious diseases to prevent spread, while seclusion has involved confining individuals, often in psychiatric settings, to manage behavioral crises. Your understanding of these terms benefits from recognizing how cultural and medical practices shaped their application, reflecting shifts in ethical standards and patient rights over time.
Core Differences: Isolation vs Seclusion
Isolation involves separating an individual from others due to medical or safety reasons, often to prevent infection spread or protect the person. Seclusion refers to confining someone alone in a room or area as a behavioral control measure, typically used in psychiatric or correctional settings. Understanding your rights and context around these terms ensures appropriate application and safeguards personal dignity.
Psychological Impacts of Isolation
Isolation, seclusion, and quarantine differ primarily in context and purpose, with isolation specifically referring to separating individuals with contagious conditions to prevent disease spread. Psychological impacts of isolation include increased risks of anxiety, depression, and cognitive decline due to extended social disconnection and sensory deprivation. Research indicates that prolonged isolation can exacerbate mental health disorders and impair emotional regulation, emphasizing the need for supportive interventions.
Psychological Effects of Seclusion
Seclusion in mental health settings involves forcibly isolating an individual, often leading to increased anxiety, depression, and post-traumatic stress symptoms due to the imposed loss of control and social contact. Unlike voluntary isolation, seclusion triggers heightened psychological distress and feelings of helplessness, potentially exacerbating pre-existing mental health conditions. Research underscores the importance of minimizing seclusion practices to prevent long-term emotional and cognitive impairments in vulnerable patients.
Isolation and Seclusion in Healthcare Settings
Isolation in healthcare settings refers to the separation of patients with contagious diseases to prevent the spread of infection, using specific protocols and protective measures. Seclusion involves confining a patient alone in a room or area for safety reasons, usually to manage acute behavioral disturbances, and is governed by strict legal and ethical guidelines. Your understanding of these practices is crucial to ensuring patient safety while respecting dignity and rights during treatment.
Legal and Ethical Considerations
Legal and ethical considerations around isolation, seclusion, and quarantine focus on protecting individual rights while ensuring public safety. You must understand that isolation legally refers to separating individuals diagnosed with contagious diseases, seclusion involves confining a person, often in a behavioral health setting, as a safety measure, and quarantine restricts movement of those exposed but not yet symptomatic. Ethics demand minimizing harm, securing informed consent when possible, and ensuring conditions respect dignity and provide necessary care to individuals during these restrictive measures.
Best Practices for Prevention and Alternatives
Isolation, seclusion, and restraint are distinct interventions used in behavioral health with critical safety considerations and ethical implications. Best practices for prevention include implementing comprehensive staff training on de-escalation techniques, creating individualized behavior support plans, and ensuring environments that reduce sensory overload. Alternatives to these practices involve utilizing positive behavioral interventions, enhancing communication strategies, and promoting trauma-informed care to prevent situations that trigger the need for isolation or seclusion.
Case Studies: Real-World Applications
Case studies reveal distinct applications of isolation, seclusion, and quarantine in healthcare and correctional settings, highlighting isolation primarily used for infectious disease control, seclusion implemented for behavioral management in psychiatric units, and quarantine applied during outbreaks to prevent disease spread. Research indicates isolation reduces nosocomial infections in hospital environments, while seclusion limits harm by restricting movement of aggressive patients. Quarantine enforcement during epidemics, such as COVID-19, demonstrates effectiveness in containing transmission within communities and limiting public health crises.
Conclusion: Making Informed Decisions
Isolation involves separating individuals to prevent disease spread, often used in healthcare settings; seclusion is a behavioral intervention used primarily in psychiatric care to manage disruptive behavior by placing a person alone in a controlled environment. Making informed decisions requires understanding the distinct purposes, ethical considerations, and legal regulations governing each practice to ensure patient safety and rights are upheld. Clear criteria and multidisciplinary approaches optimize outcomes while minimizing negative psychological impacts associated with prolonged confinement.
Infographic: Isolation vs Seclusion
 relatioo.com
relatioo.com