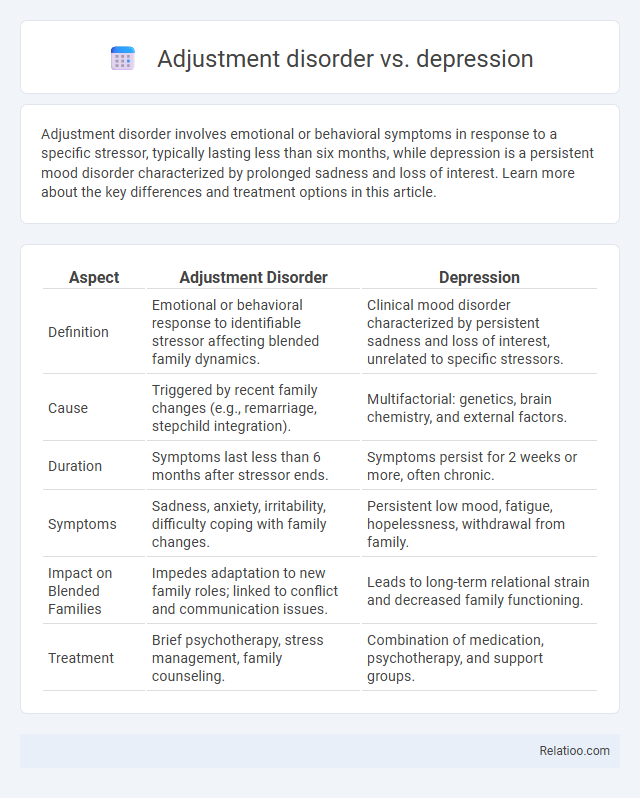
Adjustment disorder involves emotional or behavioral symptoms in response to a specific stressor, typically lasting less than six months, while depression is a persistent mood disorder characterized by prolonged sadness and loss of interest. Learn more about the key differences and treatment options in this article.
Table of Comparison
| Aspect | Adjustment Disorder | Depression |
|---|---|---|
| Definition | Emotional or behavioral response to identifiable stressor affecting blended family dynamics. | Clinical mood disorder characterized by persistent sadness and loss of interest, unrelated to specific stressors. |
| Cause | Triggered by recent family changes (e.g., remarriage, stepchild integration). | Multifactorial: genetics, brain chemistry, and external factors. |
| Duration | Symptoms last less than 6 months after stressor ends. | Symptoms persist for 2 weeks or more, often chronic. |
| Symptoms | Sadness, anxiety, irritability, difficulty coping with family changes. | Persistent low mood, fatigue, hopelessness, withdrawal from family. |
| Impact on Blended Families | Impedes adaptation to new family roles; linked to conflict and communication issues. | Leads to long-term relational strain and decreased family functioning. |
| Treatment | Brief psychotherapy, stress management, family counseling. | Combination of medication, psychotherapy, and support groups. |
Understanding Adjustment Disorder
Adjustment disorder involves emotional or behavioral symptoms triggered by a specific stressor, differing from depression, which is characterized by persistent feelings of sadness and loss of interest without a clear external cause. Your ability to recognize adjustment disorder early can lead to effective coping strategies and prevent progression to more severe mental health conditions. Treatment often includes therapy and stress management techniques tailored to your unique situation.
Defining Depression
Depression is a mood disorder characterized by persistent feelings of sadness, hopelessness, and a lack of interest or pleasure in daily activities, significantly impairing Your ability to function. Adjustment disorder, often confused with depression, occurs as a response to a specific stressor and typically resolves once the stressor is removed or coping improves. Understanding the clinical differences between depression and adjustment disorder is essential for accurate diagnosis and effective treatment planning.
Key Differences Between Adjustment Disorder and Depression
Adjustment disorder and depression share overlapping symptoms such as sadness and withdrawal, but key differences lie in their causes and duration. Adjustment disorder typically arises from a specific stressful event and resolves within six months once you adapt, whereas depression is a persistent medical condition that can occur without a clear trigger and last much longer. Your treatment approach will vary, with adjustment disorder often responding well to therapy aimed at coping strategies, while depression may require a combination of medication and psychotherapy.
Common Symptoms Compared
Adjustment disorder and depression share several common symptoms, including persistent sadness, tearfulness, and difficulty concentrating, which affect Your daily functioning. Both conditions may involve feelings of hopelessness, changes in sleep patterns, and irritability, but adjustment disorder symptoms typically arise in response to identifiable stressors and are time-limited. Unlike depression, adjustment disorder symptoms often improve once the stressor is removed or adapted to, whereas depression may require longer-term treatment and can occur without a specific trigger.
Causes and Triggers: Adjustment Disorder vs Depression
Adjustment disorder is primarily triggered by identifiable external stressors such as job loss, relationship problems, or major life changes, causing emotional or behavioral symptoms. Depression often arises due to a combination of genetic, biochemical, environmental, and psychological factors, with symptoms persisting independently of a specific external event. Unlike depression, adjustment disorder symptoms occur within three months of the stressor and typically improve once the stressor is removed or resolved.
Diagnostic Criteria Overview
Adjustment disorder is characterized by emotional or behavioral symptoms in response to a specific identifiable stressor, occurring within three months of the stressor and lasting no longer than six months after its removal. Depression involves persistent sadness or loss of interest, accompanied by at least five symptoms such as changes in sleep, appetite, energy, and feelings of worthlessness, lasting for at least two weeks and causing significant impairment. Differentiating adjustment disorder from depression relies on the presence of a clear stressor, symptom severity, duration, and whether the symptoms meet full criteria for major depressive disorder as outlined in the DSM-5.
Treatment Approaches: Similarities and Differences
Treatment approaches for adjustment disorder primarily involve psychotherapy, particularly cognitive-behavioral therapy (CBT), aimed at managing stressors and improving coping skills, whereas depression often requires a combination of antidepressant medications and psychotherapy to address chemical imbalances and persistent mood disturbances. Both conditions benefit from supportive counseling and psychoeducation, but adjustment disorder treatments typically have a shorter duration due to the situational nature of the disorder, while depression treatment may be longer and more intensive. In cases where adjustment disorder coexists with depression, integrated treatment plans combining pharmacotherapy and psychotherapy are necessary to effectively address overlapping symptoms and functional impairments.
Impact on Daily Life
Adjustment disorder causes emotional or behavioral symptoms that interfere with daily functioning but often improve once the stressor is resolved, affecting work, social activities, and relationships temporarily. Depression leads to persistent feelings of sadness, loss of interest, and fatigue, significantly impairing daily life across multiple domains such as concentration, motivation, and physical health. Compared to depression, adjustment disorder's impact on daily life is usually less severe and shorter in duration but still disrupts routine activities and overall well-being during stressful periods.
When to Seek Professional Help
Seek professional help if symptoms of adjustment disorder persist beyond six months or significantly interfere with daily functioning, such as work or relationships. Depression requires immediate attention when experiencing prolonged sadness, loss of interest, or suicidal thoughts, indicating the need for a comprehensive mental health evaluation. Differentiating between adjustment disorder and depression is crucial as both involve mood disturbances but vary in severity and treatment urgency.
Coping Strategies and Support Systems
Adjustment disorder involves difficulty coping with a specific stressor, while depression is characterized by pervasive low mood and loss of interest beyond situational triggers. Effective coping strategies for adjustment disorder include stress management techniques and seeking social support, whereas depression often requires a combination of therapy, medication, and strong support networks. Your ability to engage in healthy coping mechanisms and utilize support systems can significantly impact recovery from both conditions.
Infographic: Adjustment disorder vs Depression
 relatioo.com
relatioo.com