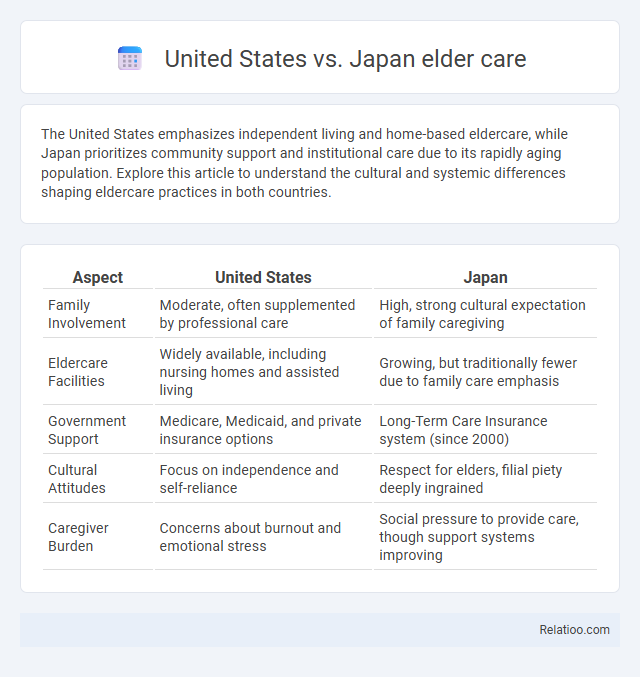
The United States emphasizes independent living and home-based eldercare, while Japan prioritizes community support and institutional care due to its rapidly aging population. Explore this article to understand the cultural and systemic differences shaping eldercare practices in both countries.
Table of Comparison
| Aspect | United States | Japan |
|---|---|---|
| Family Involvement | Moderate, often supplemented by professional care | High, strong cultural expectation of family caregiving |
| Eldercare Facilities | Widely available, including nursing homes and assisted living | Growing, but traditionally fewer due to family care emphasis |
| Government Support | Medicare, Medicaid, and private insurance options | Long-Term Care Insurance system (since 2000) |
| Cultural Attitudes | Focus on independence and self-reliance | Respect for elders, filial piety deeply ingrained |
| Caregiver Burden | Concerns about burnout and emotional stress | Social pressure to provide care, though support systems improving |
Introduction to Eldercare Systems in the United States and Japan
The United States eldercare system emphasizes a combination of private and public services, including Medicare and Medicaid funding, home health care, assisted living, and nursing facilities, targeting diverse aging populations. Japan's eldercare system is structured around its Long-Term Care Insurance (LTCI), which provides universal coverage with a focus on community-based services, rehabilitation, and family support due to its rapidly aging society. Both countries prioritize improving quality of life, but Japan's model relies more heavily on government-managed programs, whereas the U.S. system integrates private-sector providers extensively.
Demographic Trends Influencing Eldercare
The United States faces a rapidly aging population with a significant rise in seniors requiring long-term care, driven by increased life expectancy and declining birth rates. Japan's eldercare system is under immense pressure due to the world's highest proportion of people aged 65 and older, leading to innovative policies and a growing reliance on robotics and community-based care. Your understanding of these demographic trends highlights key differences in how each country addresses the challenges of an aging society and the growing demand for eldercare services.
Government Policies and Funding for Eldercare
The United States allocates significant federal funding to eldercare through programs like Medicare and Medicaid, emphasizing home- and community-based services, while Japan's government implements long-term care insurance (LTCI) established in 2000 to cover eldercare comprehensively for those aged 65 and older. Japan's LTCI system is funded through mandatory contributions from citizens and local government subsidies, ensuring widespread access to institutional and community-based care. In contrast, U.S. eldercare policies rely heavily on state-administered programs and private insurance, resulting in a less uniform, market-driven funding landscape.
Family Roles and Cultural Expectations in Eldercare
In the United States, eldercare often emphasizes individualism, with families relying on formal care services and institutional support for aging relatives, reflecting a cultural expectation of independence. Japan's eldercare system is deeply rooted in Confucian values, where family members, especially daughters-in-law, are traditionally expected to provide hands-on care, highlighting strong filial piety and multigenerational living arrangements. Your approach to eldercare may vary greatly depending on cultural norms, with American families balancing professional assistance and personal involvement, while Japanese families prioritize familial responsibility and respect for elder authority.
Types of Eldercare Services Offered
In the United States, eldercare services primarily include in-home care, assisted living facilities, and nursing homes, emphasizing personalized care and medical support. Japan focuses on long-term care insurance systems, offering community-based services, day care centers, and institutional care tailored to the aging population. Your choice between US and Japanese eldercare may depend on the types of services prioritized in each country, such as the US's emphasis on diverse living arrangements versus Japan's integrated insurance and community care models.
Workforce Challenges in Eldercare
The United States faces a significant eldercare workforce shortage, with over 2.5 million direct care jobs expected to open by 2030, driven by aging populations and high turnover rates. Japan, confronting the world's fastest aging society, struggles with a shrinking labor pool and increasing demand, prompting innovations like robotics and foreign caregiver programs to supplement human resources. Both countries grapple with challenges including low wages, demanding workload conditions, and the need for comprehensive training to sustain quality eldercare services.
Technology and Innovation in Eldercare Solutions
The United States leads in eldercare technology with advanced AI-driven monitoring systems and smart home integrations, enhancing patient safety and autonomy. Japan excels in robotic care innovations, deploying companion robots and automated mobility aids to address its rapidly aging population. Both countries prioritize telehealth platforms and wearable health devices to improve healthcare accessibility and real-time eldercare management.
Quality of Life and Wellbeing of Older Adults
The United States emphasizes individualized eldercare approaches that prioritize autonomy and access to advanced medical technology, enhancing the quality of life and wellbeing of older adults. Japan integrates community-based support and traditional family caregiving, promoting social inclusion and mental health among its elderly population. You can benefit from understanding these contrasting models to tailor eldercare solutions that maximize both physical and emotional wellbeing.
Financial Costs and Accessibility of Eldercare
Eldercare in the United States often involves higher financial costs due to extensive use of private facilities and insurance-based payment systems, whereas Japan benefits from a robust public long-term care insurance program that helps lower out-of-pocket expenses for seniors. Accessibility to eldercare services in Japan is generally more widespread due to government policies promoting community-based care and aging in place, while in the U.S., geographic disparities and insurance coverage gaps can limit your access to quality eldercare. Understanding these financial and accessibility differences can help you navigate options effectively when planning for eldercare needs.
Future Prospects and Emerging Trends in Eldercare
The United States and Japan showcase contrasting future prospects in eldercare, with the U.S. emphasizing technology-driven solutions like AI and remote monitoring to address a growing aging population. Japan leads in robotic care and community-based eldercare models, driven by its higher elderly demographic and workforce shortages. Emerging trends include personalized care platforms, integration of IoT devices for health tracking, and expansion of telehealth services to enhance quality and accessibility in both countries.
Infographic: United States vs Japan eldercare
 relatioo.com
relatioo.com